What Is Pancreatitis and How Does It Affect Your Health?
Pancreatitis is the inflammation of the pancreas, causing symptoms like severe abdominal pain, nausea, and vomiting. It can be triggered by factors such as gallstones, excessive alcohol consumption, or certain medications. Left untreated, pancreatitis can lead to serious complications. At Digestive Disease Care, Dr. Nilesh Mehta, MD, and our team of board-certified gastroenterologists offer specialized care tailored to your needs, providing accurate diagnosis and personalized treatment options to effectively manage pancreatitis and enhance your quality of life. For more information, contact us today or schedule an appointment online. We have convenient locations to serve you in Babylon NY, East Setauket NY, Forest Hills NY, Jericho NY, Lake Success NY, Melville NY, Mineola NY, Massapequa NY, New Hyde Park NY, and Riverhead NY.
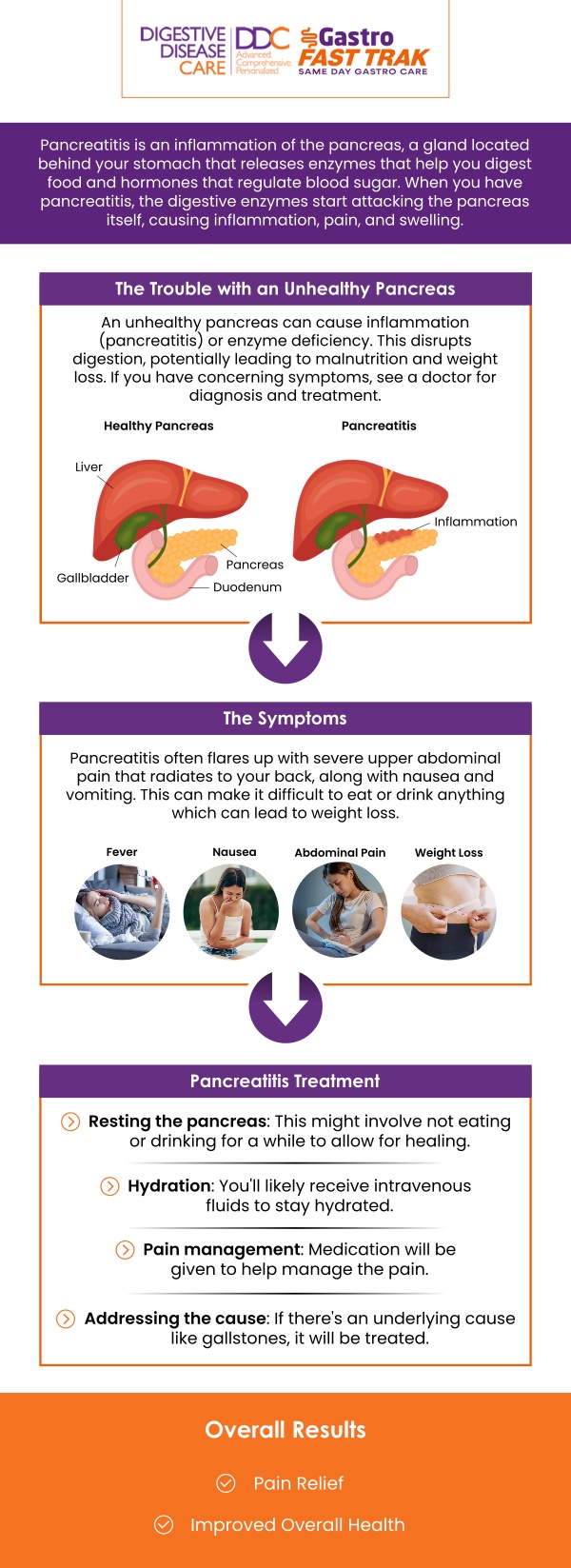
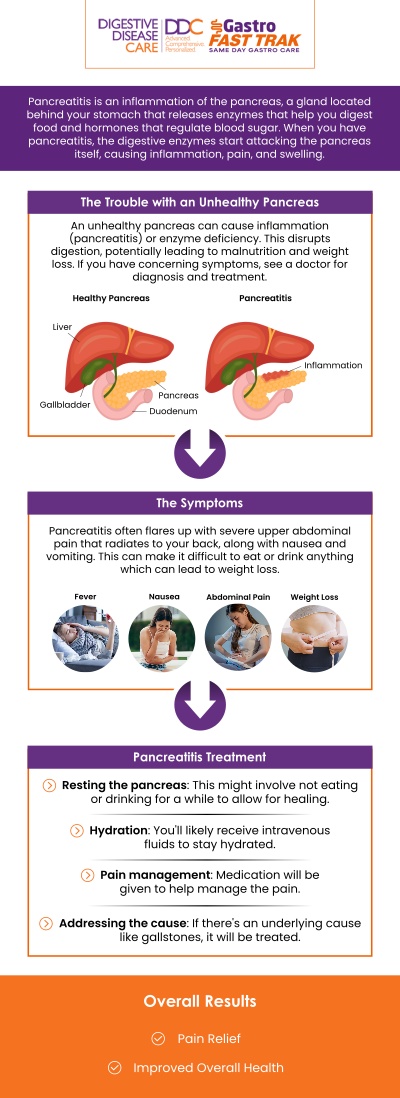
Table of Contents:
What causes pancreatitis, and how does it develop?
How does pancreatitis impact blood sugar levels?
What are the long-term effects of chronic pancreatitis on health?
How does pancreatitis affect your nutritional intake?
Dr. Preeti Mehta, MD at Digestive Disease Care: Everything You Need to Know About Pancreatitis
Pancreatitis is the inflammation of the pancreas, a crucial organ responsible for producing digestive enzymes and hormones like insulin. It can develop suddenly (acute pancreatitis) or as a long-term condition (chronic pancreatitis). Here’s an overview of the causes and how pancreatitis develops:
1. Gallstones
One of the most common causes of pancreatitis is gallstones, which can block the bile duct. When the bile duct becomes blocked, digestive enzymes back up into the pancreas, leading to inflammation and potential damage.
2. Chronic Alcohol Consumption
Heavy and prolonged alcohol use is another major cause of pancreatitis. Alcohol can irritate the pancreas, causing inflammation and impairing its ability to secrete digestive enzymes properly. Over time, this can lead to chronic pancreatitis.
3. High Blood Triglycerides
Elevated triglyceride levels in the blood can increase the risk of pancreatitis. High triglycerides can cause the pancreas to become inflamed and may lead to an acute episode of pancreatitis.
4. Medications
Certain medications can trigger pancreatitis as a side effect. Drugs used to treat conditions like high cholesterol, autoimmune diseases, and infections may contribute to inflammation in the pancreas.
5. Abdominal Injury or Surgery
Injury to the abdomen, particularly the pancreas, can lead to inflammation. Additionally, complications from abdominal surgery may cause damage to the pancreas, resulting in pancreatitis.
6. Genetic Factors
In some cases, pancreatitis can be inherited due to genetic mutations. These inherited forms of pancreatitis can cause chronic inflammation and damage to the pancreas over time.
7. Infections and Other Medical Conditions
Viral infections, such as mumps or hepatitis, can lead to pancreatitis. Conditions like cystic fibrosis and high calcium levels in the blood can also contribute to its development.
Understanding the causes of pancreatitis is essential for early detection and management. If you experience persistent abdominal pain or other symptoms, consult Dr. Nilesh Mehta, MD, and our team of board-certified gastroenterologists at Digestive Disease Care for proper diagnosis and treatment options.
Pancreatitis can significantly impact blood sugar levels due to its effect on the pancreas, which plays a key role in regulating glucose. Here’s how pancreatitis can affect blood sugar:
• Impaired Insulin Production: The pancreas produces insulin, which helps regulate blood sugar. Inflammation from pancreatitis can damage the insulin-producing cells, leading to reduced insulin production. This can result in high blood sugar (hyperglycemia) as the body struggles to process glucose.
• Increased Risk of Diabetes: Chronic pancreatitis, which involves long-term inflammation, can cause lasting damage to the pancreas, impairing its ability to produce insulin. Over time, this increases the risk of developing type 1 or type 2 diabetes, with persistent high blood sugar levels requiring ongoing management.
• Insulin Resistance: Pancreatitis can contribute to insulin resistance, where the body’s cells become less responsive to insulin. This can result in higher blood sugar levels as more insulin is needed to regulate glucose.
• Blood Sugar Fluctuations in Acute Pancreatitis: In acute pancreatitis, blood sugar levels can fluctuate due to stress, inflammation, or complications. Blood sugar may temporarily increase, especially in individuals who already have diabetes or other metabolic issues, requiring careful monitoring and management.
• Nutrient Malabsorption: Pancreatitis can affect the absorption of essential nutrients, which can disrupt overall metabolic functions, including blood sugar regulation. This can make blood sugar control more difficult, especially for those with pre-existing conditions like diabetes.
If you are experiencing pancreatitis or blood sugar fluctuations, it’s important to consult a healthcare provider. Dr. Nilesh Mehta, MD, and our team of board-certified gastroenterologists at Digestive Disease Care are here to provide expert care and help manage both pancreatitis and blood sugar levels effectively.
Chronic pancreatitis is a long-term inflammation of the pancreas that can lead to permanent damage and serious health complications. Over time, the pancreas loses its ability to function properly, which can have wide-reaching effects on your health. Here are some key long-term effects of chronic pancreatitis:
• Impaired Digestive Function: As chronic pancreatitis progresses, the pancreas becomes less able to produce digestive enzymes. This can lead to malabsorption of nutrients, resulting in weight loss, vitamin deficiencies, and digestive problems like diarrhea and bloating.
• Diabetes: The pancreas also produces insulin, which helps regulate blood sugar. Damage to insulin-producing cells can lead to diabetes, particularly type 3c diabetes, which is directly related to pancreatic dysfunction. People with chronic pancreatitis are at a higher risk of developing diabetes over time.
• Chronic Pain: One of the most debilitating long-term effects of chronic pancreatitis is persistent abdominal pain. This pain can range from mild to severe and is often worsened by eating, particularly high-fat meals. This ongoing discomfort can significantly impact quality of life.
• Pancreatic Cancer: Chronic pancreatitis increases the risk of pancreatic cancer. Long-term inflammation can lead to the formation of abnormal cells that may eventually develop into cancer. Regular monitoring is necessary for those with chronic pancreatitis to detect any early signs of cancer.
• Nutritional Deficiencies: Due to malabsorption, individuals with chronic pancreatitis are at risk of deficiencies in vitamins such as A, D, E, and K, as well as minerals like calcium and magnesium. This can lead to further health complications like bone loss or anemia.
If you are managing chronic pancreatitis, it is essential to work with a healthcare provider like Dr. Nilesh Mehta, MD, and our team of board-certified gastroenterologists at Digestive Disease Care. Early intervention and proper care can help manage symptoms and reduce the risk of long-term complications.
Pancreatitis can significantly impact your nutritional intake due to the pancreas’s role in producing digestive enzymes and regulating blood sugar. Here are some key ways pancreatitis affects nutrition:
• Impaired Digestion and Malabsorption: The pancreas produces enzymes that are essential for breaking down fats, proteins, and carbohydrates in food. When pancreatitis causes inflammation, the pancreas may not produce enough of these enzymes, leading to malabsorption of nutrients. This means your body struggles to absorb essential vitamins and minerals from food, resulting in weight loss and nutritional deficiencies.
• Fat Malabsorption: Chronic pancreatitis can cause difficulty in digesting fats. As a result, people with pancreatitis may experience steatorrhea, which is the presence of undigested fat in the stool. This can lead to diarrhea, bloating, and deficiencies in fat-soluble vitamins (A, D, E, and K).
• Reduced Appetite: Pancreatitis often causes discomfort, including abdominal pain and nausea, which can lead to a reduced appetite. This makes it challenging to consume enough food to meet your daily nutritional needs, further contributing to malnutrition.
• Vitamin and Mineral Deficiencies: As a result of malabsorption, people with pancreatitis may become deficient in important nutrients, including vitamin D, calcium, magnesium, and B12. These deficiencies can lead to bone loss, muscle weakness, and other health issues.
• Blood Sugar Imbalance: If pancreatitis leads to damage of insulin-producing cells in the pancreas, it can cause diabetes or insulin resistance. This can affect the body’s ability to process nutrients properly, leading to challenges in maintaining stable blood sugar levels and requiring adjustments in diet.
At Digestive Disease Care, Dr. Nilesh Mehta, MD, and our team of board-certified gastroenterologists specialize in managing pancreatitis and its impact on nutrition. We provide comprehensive care to help you manage symptoms, improve digestion, and ensure you get the nutrients your body needs.
Pancreatitis is a serious condition that causes inflammation of the pancreas, leading to symptoms such as severe abdominal pain, nausea, vomiting, and digestive issues. At Digestive Disease Care, Dr. Preeti Mehta, MD, and our team of board-certified gastroenterologists provide expert care for both acute and chronic pancreatitis. Early detection and proper management are crucial to reducing complications and improving quality of life. Whether you’re dealing with sudden symptoms or managing chronic pancreatitis, Dr. Mehta offers comprehensive evaluation and personalized treatment plans to meet your specific needs.
At Digestive Disease Care, we understand the impact of pancreatitis on your health. Our state-of-the-art diagnostic tools, including blood tests and imaging, allow Dr. Preeti Mehta, MD, to accurately diagnose the severity of the condition and provide timely interventions. We focus on managing symptoms, improving digestive function, and preventing complications like diabetes or pancreatic cancer. If you’re experiencing symptoms of pancreatitis or need ongoing care, schedule an appointment with Dr. Mehta and our team for the expert care you deserve. For more information, contact us today or schedule an appointment online. We have convenient locations to serve you in Babylon NY, East Setauket NY, Forest Hills NY, Jericho NY, Lake Success NY, Melville NY, Mineola NY, Massapequa NY, New Hyde Park NY, and Riverhead NY.

Check Out Our 5 Star Reviews


Additional Services You May Like

Additional Services You May Like
- Abdominal Pain
- Acid Reflux
- Barretts Esophagus
- Bloating
- Capsule Endoscopy
- Celiac Disease
- Colon Cancer Screening
- Colonoscopy
- Constipation
- Crohns Disease
- Diarrhea
- Diverticulitis
- Esophageal PH Monitoring
- Fatty Liver
- Fibroscan
- Gallstones
- Gastroenterologist
- Gastric Chest Pain
- Gluten Intolerance
- Hemorrhoid
- Hemorrhoid Banding
- Hepatitis
- Irritable Bowel Syndrome
- Lactose Intolerance
- Pancreatitis
- Polyps
- Rectal Bleeding
- Stomach
- Ulcerative Colitis
- GI Urgent Care





