Ulcerative Colitis – Symptoms and Causes
At Digestive Disease Care (DDC), our board-certified gastroenterologists provide diagnosis and management of ulcerative colitis. This chronic inflammatory bowel disease causes symptoms like abdominal pain, diarrhea with blood, and weight loss. The exact cause is unknown, but it may involve an overactive immune response, genetics, and environmental factors, potentially leading to complications like anemia, dehydration, and an increased risk of colon cancer. For more information, contact us or book an appointment online. We have convenient locations to serve you in Babylon NY, East Setauket NY, Forest Hills NY, Jericho NY, Lake Success NY, Melville NY, Mineola NY, Massapequa NY, New Hyde Park NY and Riverhead NY.
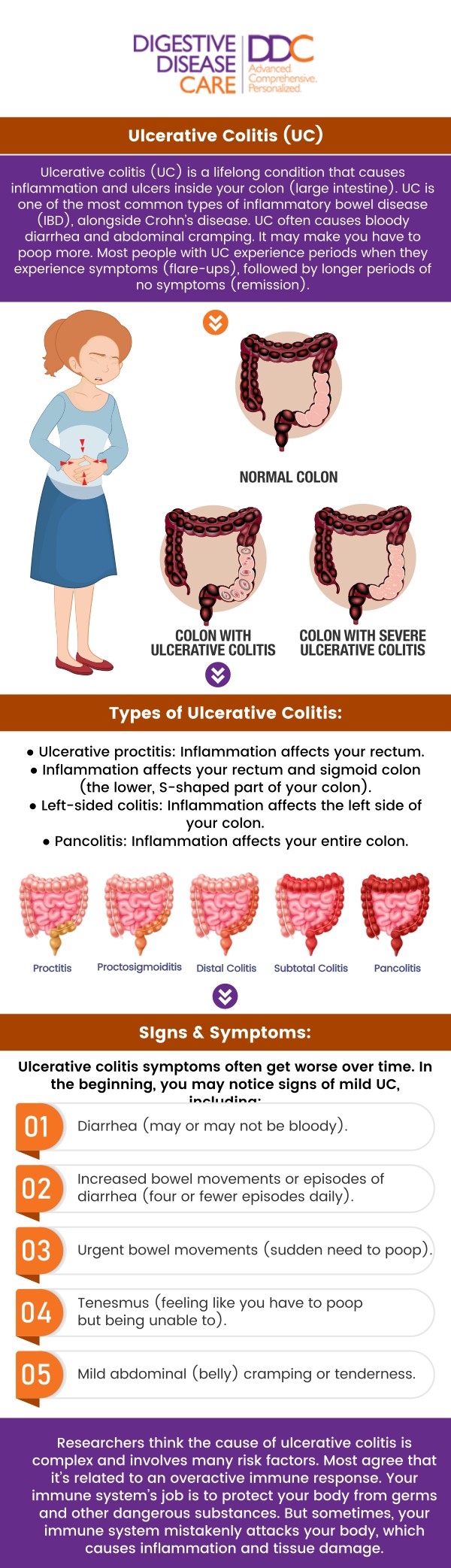
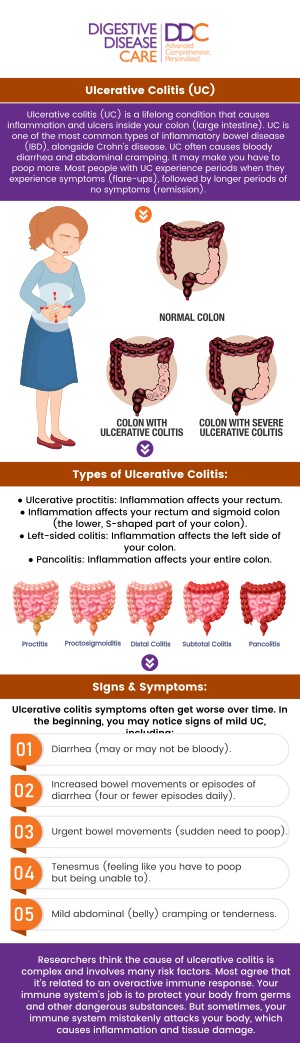


Table of Contents:
What are the symptoms of ulcerative colitis?
What triggers ulcerative colitis flare-ups?
How is ulcerative colitis diagnosed?
How often should I see a doctor for ulcerative colitis?
Ulcerative colitis is a chronic inflammatory bowel disease that affects the lining of the large intestine and rectum. This condition exhibits a range of symptoms, including a progressive loosening of stool, abdominal pain, cramping, decreased appetite, and weight loss, among others. These symptoms can greatly vary among our patients, sometimes being mild and at other times severe enough to interfere with daily activities.
We understand that frequent bowel movements, which are often a result of ulcerative colitis, can lead to significant fluid loss and dehydration. In certain severe instances, our patients may also experience rectal bleeding.
Our team of board-certified gastroenterologists is equipped to handle the abdominal pain and cramping associated with this disease. We monitor these symptoms, which can be intermittent or constant, and may worsen after eating or as the day progresses.
The damage caused by ulcerative colitis to the colon often leads to malnutrition, as the colon plays a crucial role in absorbing key nutrients. This can further lead to reduced appetite and weight loss. We also look out for fatigue, which can be a result of the body’s energy being used to fight inflammation, or anemia caused by blood loss in stool.
Patients with ulcerative colitis often suffer from abdominal pain, diarrhea, bloody stools, and fatigue. While the exact cause remains unknown, various factors can trigger flare-ups or exacerbate symptoms.
Stress is a primary trigger for many of our patients. We see a common trend of symptoms worsening during periods of high stress or tension. This is why we often incorporate stress management techniques into our treatment plans, helping control the frequency and severity of flare-ups.
Dietary factors are also significant in managing this condition. Although no specific food or group of foods is known to cause ulcerative colitis, certain types can worsen symptoms. These include dairy products, gluten, spicy dishes, high-fat foods, high-fiber foods, artificial sweeteners, and sugar alcohols, especially in those with lactose intolerance.
Lifestyle factors such as smoking and lack of sleep can exacerbate symptoms. At our practice, we encourage healthy lifestyle habits as part of managing this condition. Certain medications, infections, hormonal changes, and even weather changes can trigger flare-ups.
Triggers for ulcerative colitis can vary greatly between individuals. What bothers one patient may not affect another. We believe in a tailored approach, carefully considering each patient’s unique symptoms and triggers. We foster open dialogue and teamwork to proactively prevent and manage flare-ups.
We have a team of experienced gastroenterologists who specialize in diagnosing and treating conditions such as ulcerative colitis. We understand that diagnosing this condition can be complex, as there is no single definitive test for ulcerative colitis.
This is why our approach includes a comprehensive assessment that begins with a thorough physical examination and a detailed review of your medical history. We take into account your symptoms, such as diarrhea, abdominal pain, or weight loss, and the duration of your illness. Our gastroenterologists conduct a visual inspection of the anal area and a gentle digital rectal examination to assess for inflammation and tenderness.
We also consider crucial factors such as a family history of ulcerative colitis or other inflammatory bowel diseases. Once the initial review is done, we conduct necessary blood tests to reveal signs of inflammation. These blood tests can also detect anemia or electrolyte imbalances, which may suggest ulcerative colitis.
In addition to blood tests, we analyze stool samples to check for the presence of blood, mucus, or parasites. By doing so, we can rule out other disorders like infections or parasites that may mimic ulcerative colitis symptoms.
One of the most reliable diagnostic procedures we employ is colonoscopy, which is considered the gold standard test for ulcerative colitis. During this procedure, our skilled gastroenterologists insert a thin, flexible tube with a camera into the rectum and colon, allowing us to visualize the lining of these organs and look for inflammation, bleeding, or ulcers.
The biopsies obtained during an endoscopy are examined under a microscope. They look for characteristic changes in the cells and tissue architecture that indicate the presence of ulcerative colitis.
In some cases, additional imaging tests like X-rays or CT scans may be needed. These tests provide images of the colon and the surrounding structures, helping us detect complications like a perforated colon.
The frequency of these visits will significantly depend on several factors, including the severity of the UC, the efficiency of the treatment plan, and individual patient factors such as age and overall health.
Our patients with mild to moderate UC may need to see our specialized gastroenterologists every 3-6 months for routine monitoring. These regular check-ups usually involve physical exams, blood tests, and stool analysis to assess the disease activity and the patient’s overall health. Patients whose UC is well-managed and are not witnessing any significant symptoms might only require an annual check-up.
We prioritize patient health, hence more frequent visits are necessitated during active flare-ups, which are periods when the symptoms worsen. During these times, visits may occur weekly or even more often, as our doctors need to closely monitor the symptoms, adjust medications, and provide supportive care to manage the inflammation and reduce discomfort.
For newly diagnosed patients or those starting a new treatment for UC, our doctors may want to see them more frequently initially. This is to ensure the medication’s effectiveness, monitor for potential side effects, and adjust the treatment plan as needed. The frequency of these visits will gradually decrease as the condition stabilizes and improves.
We also understand that patients with ulcerative colitis are at an increased risk of colon cancer. Therefore, regular screening for colon cancer is recommended at our medical practice, usually starting 8 to 10 years after the diagnosis of UC.
Regardless of the patient’s condition, skipping regular appointments is not advisable. Even when the condition is well-controlled, routine check-ups are a key part of managing ulcerative colitis and maintaining a good quality of life.
At Digestive Disease Care, our team is always ready to provide urgent medical attention if you experience any of the following symptoms: severe abdominal pain or cramping, bloody diarrhea, or vomiting. Schedule your consultation today and embark on a path to better health and well-being. We have convenient locations to serve you in Melville NY, New Hyde Park NY, Forest Hills NY, Jericho NY, Mineola NY, Lake Success NY, Babylon NY, East Setauket NY, Massapequa NY, Riverhead NY and BEYOND.

Check Out Our 5 Star Reviews


Additional Services You May Like

Additional Services You May Like
- Abdominal Pain
- Acid Reflux
- Barretts Esophagus
- Bloating
- Capsule Endoscopy
- Celiac Disease
- Colon Cancer Screening
- Colonoscopy
- Constipation
- Crohns Disease
- Diarrhea
- Diverticulitis
- Esophageal PH Monitoring
- Fatty Liver
- Fibroscan
- Gallstones
- Gastroenterologist
- Gastric Chest Pain
- Gluten Intolerance
- Hemorrhoid
- Hemorrhoid Banding
- Hepatitis
- Irritable Bowel Syndrome
- Lactose Intolerance
- Pancreatitis
- Polyps
- Rectal Bleeding
- Stomach
- Ulcerative Colitis
- GI Urgent Care





