Diverticulitis Treatment Specialist in East Setauket, NY
Diverticulitis is a condition where small pouches in the colon become inflamed or infected, causing symptoms like abdominal pain, fever, and changes in bowel movements. It can lead to serious complications if left untreated, such as abscesses or bowel perforation. At Digestive Disease Care, our board-certified gastroenterologists provide specialized diagnosis and treatment to manage diverticulitis and alleviate symptoms effectively. For more information, contact us today or schedule an appointment online. We are conveniently located at 235 N Belle Mead Rd, East Setauket, NY 11733.
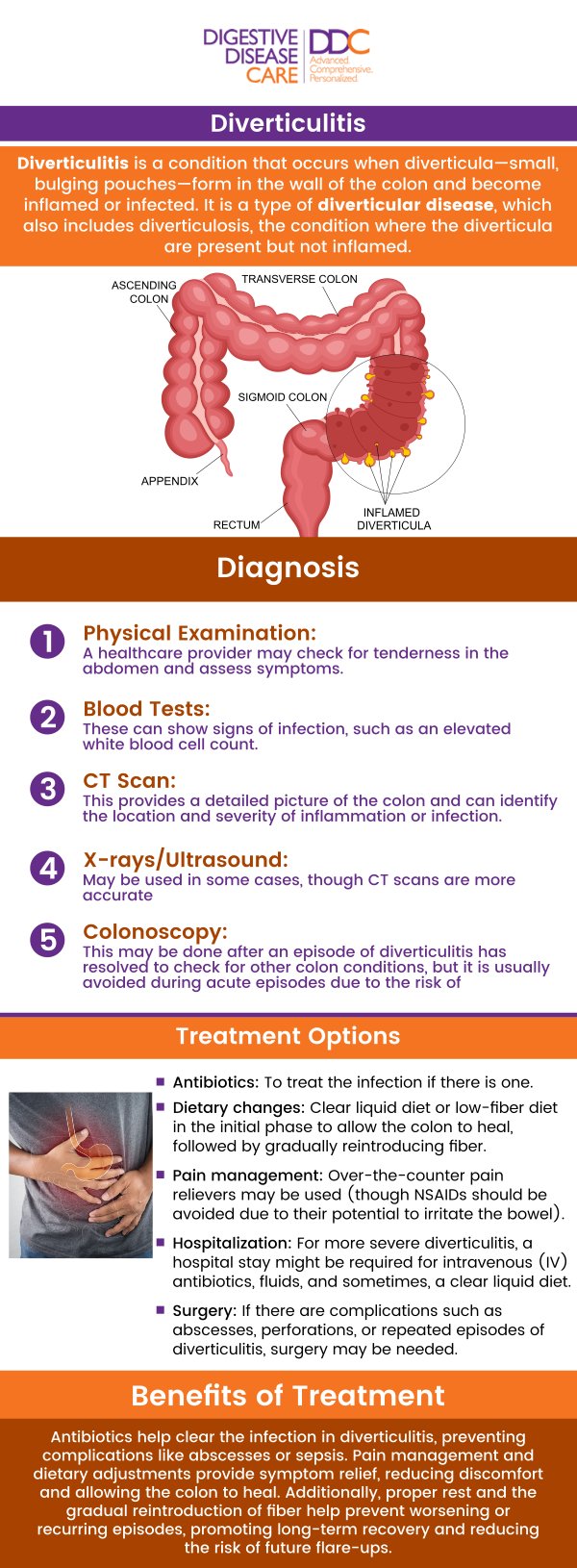
Table of Contents:
How is diverticulitis diagnosed?
What are the different stages of diverticulitis?
Is diverticulitis a chronic condition?
When should I see a doctor for diverticulitis?
Diverticulitis is diagnosed through a combination of medical history, physical examination, and imaging tests. The doctor will typically assess the patient’s symptoms and may perform specific tests to confirm the diagnosis and determine the severity of the condition.
How Diverticulitis is Diagnosed:
1. Medical History and Symptoms Review
The doctor will first ask about your symptoms, including abdominal pain, changes in bowel habits, fever, nausea, or vomiting. A thorough review of your medical history will also be conducted to assess risk factors, such as diet, lifestyle, and any previous gastrointestinal issues.
2. Physical Examination
During a physical exam, the doctor may press on the abdomen to check for areas of tenderness or pain, particularly in the lower left side, which is the common location for diverticulitis. The doctor may also look for signs of infection, such as fever, elevated heart rate, or abnormal bowel sounds.
3. Blood Tests
Blood tests may be ordered to check for signs of infection, such as an elevated white blood cell count, which is common in diverticulitis. These tests can also help rule out other potential causes of symptoms.
4. Imaging Tests
• CT Scan (Computed Tomography): A CT scan is the most common and accurate test used to diagnose diverticulitis. It helps identify the location and severity of the inflammation and detects any complications like abscesses or perforation.
• Ultrasound: In some cases, an abdominal ultrasound may be used, though it is less common than a CT scan for diagnosing diverticulitis.
5. Colonoscopy (Post-Acute Phase)
If diverticulitis is suspected, a colonoscopy is generally avoided during acute flare-ups due to the risk of perforation. However, once the inflammation subsides, a colonoscopy may be performed to check for diverticula or rule out other conditions.
The combination of these diagnostic methods helps doctors confirm diverticulitis and determine the appropriate treatment plan.
Diverticulitis is a condition that occurs when diverticula, small pouches that form in the walls of the colon, become inflamed or infected. The severity of diverticulitis can vary, and it is often classified into different stages based on the extent of inflammation and complications present. These stages help doctors determine the best course of treatment.
Stages of Diverticulitis:
1. Mild (Uncomplicated) Diverticulitis
This is the early stage of diverticulitis, where the inflammation or infection of the diverticula is localized and does not cause significant complications. Symptoms may include abdominal pain (usually in the lower left side), bloating, nausea, and changes in bowel habits, such as constipation or diarrhea. In many cases, mild diverticulitis can be treated with antibiotics, a clear liquid diet, and rest.
2. Severe (Complicated) Diverticulitis
In this stage, the inflammation or infection is more widespread and can lead to more serious complications.
These may include:
• Abscess Formation: A collection of pus that forms in the affected area of the colon.
• Fistula Formation: An abnormal connection between the colon and nearby organs, such as the bladder or vagina.
• Perforation: A hole in the colon that can lead to the leakage of stool and bacteria into the abdominal cavity, causing peritonitis (infection of the abdominal lining).
• Obstruction: The diverticulitis may cause a blockage in the colon, preventing normal bowel movements.
3. Treatment for severe diverticulitis typically involves hospitalization, intravenous antibiotics, and sometimes surgical intervention, especially if perforation or abscesses occur. Surgery may be necessary to remove the affected part of the colon, particularly if complications are severe.
4. Recurrent Diverticulitis
Some individuals experience repeated episodes of diverticulitis. Recurring diverticulitis can increase the risk of complications and may lead to the need for elective surgery to remove the affected section of the colon.
Each stage of diverticulitis requires different levels of medical care. Early intervention and appropriate management can prevent the progression to more severe stages.
Diverticulitis can become a chronic condition depending on the frequency and severity of episodes. Some individuals may experience a single episode that resolves with treatment, while others may have recurring flare-ups over time.
Here are the key points:
• Recurrent Episodes: Chronic diverticulitis occurs when individuals experience frequent flare-ups of symptoms such as abdominal pain, bloating, and changes in bowel habits. These recurrent episodes lead to ongoing inflammation and discomfort.
• Complications: Frequent flare-ups can cause complications such as abscesses (pockets of pus), fistulas (abnormal connections between organs), and strictures (narrowing of the colon). These complications make the condition harder to manage and may require more advanced treatments.
• Long-term Management: For those with chronic diverticulitis, long-term management strategies include dietary changes, particularly increasing fiber intake, medications to control symptoms, and regular monitoring to avoid flare-ups. This proactive approach helps prevent further complications.
• Regular Follow-ups: Individuals with chronic diverticulitis require regular follow-up with their healthcare provider to monitor the condition, adjust treatment as needed, and ensure overall health.
Overall, while diverticulitis may not always be chronic, recurring symptoms or complications require ongoing care to manage the condition effectively.
You should see a doctor for diverticulitis if you experience any symptoms of the condition, especially if they are severe or persistent. Early diagnosis and treatment can help prevent complications and ensure effective management of the condition.
Here are key situations when you should seek medical attention:
• Abdominal Pain: If you experience sudden, severe abdominal pain, especially in the lower left side of the abdomen, it could indicate diverticulitis. This pain may worsen with movement or after eating.
• Fever and Chills: Fever, along with chills, can be a sign of infection related to diverticulitis. This requires prompt medical evaluation, as it may indicate a more serious complication, such as an abscess or perforation.
• Changes in Bowel Habits: If you experience significant changes in your bowel movements, such as persistent diarrhea, constipation, or blood in your stool, it may be related to diverticulitis.
• Nausea and Vomiting: If you experience nausea or vomiting, especially if accompanied by severe abdominal pain, it could be a sign that the condition is worsening and may require urgent care.
• Difficulty Swallowing or Feeling Full: If you feel full quickly after eating or have difficulty swallowing, these symptoms may indicate diverticulitis or other complications.
If you experience any of these symptoms, it’s essential to consult a doctor to get an accurate diagnosis and appropriate treatment to prevent complications. Contact us today to schedule a consultation. We are conveniently located at 235 N Belle Mead Rd, Setauket- East Setauket, NY 11733. We serve patients from Setauket NY, Miller Place NY, Nesconset NY, Farmingville NY, Stony Brook NY, and Selden NY.

Check Out Our 5 Star Reviews


Additional Services You May Like

Additional Services You May Like
- Abdominal Pain
- Acid Reflux
- Barretts Esophagus
- Bloating
- Capsule Endoscopy
- Celiac Disease
- Colon Cancer Screening
- Colonoscopy
- Constipation
- Crohns Disease
- Diarrhea
- Diverticulitis
- Esophageal PH Monitoring
- Fatty Liver
- Fibroscan
- Gallstones
- Gastroenterologist
- Gastric Chest Pain
- Gluten Intolerance
- Hemorrhoid
- Hemorrhoid Banding
- Hepatitis
- Irritable Bowel Syndrome
- Lactose Intolerance
- Pancreatitis
- Polyps
- Rectal Bleeding
- Stomach
- Ulcerative Colitis
- GI Urgent Care





